/bc39b4a5-78a8-44ec-bff7-2da610109127.png)
Accurate Soap Note Template for Client Activities with Auditory Precision
Review Rating Score
As a healthcare professional, you understand the importance of accurate, comprehensive documentation of your client's health information. SOAP notes are a standard format for recording patient encounters that allows for clear communication between healthcare providers and ensures that all necessary information is documented. At BizzLibrary.com, we offer a SOAP note template that can help you streamline your documentation process, making it easy to keep track of your client's progress and maintain accurate records.
What is a SOAP Note?
A SOAP note is a standard method of documentation used by healthcare providers to organize information related to a patient's care. The acronym stands for Subjective, Objective, Assessment, and Plan, reflecting the four components of the note.
- Subjective: This component includes information that the patient provides about their symptoms, concerns, and goals. This may include their chief complaint, medical history, and any relevant personal information.
- Objective: The objective section incorporates measurable and observable data, such as vital signs, lab results, and physical exam findings.
- Assessment: The assessment section summarizes the healthcare provider's clinical impression of the patient's condition, including a list of differential diagnoses and a summary of the patient's progress.
- Plan: The plan section includes the healthcare provider's intended course of treatment, including medication prescriptions, diagnostic tests, referrals, and follow-up appointments.
Why Do You Need a SOAP Note Template?
SOAP notes are essential for effective communication between healthcare providers, ensuring that all members of the care team have access to the same information about the patient's progress and care plan. A well-designed SOAP note template can help you maintain complete and accurate records, improving patient safety and minimizing the risk of errors or omissions.
Our SOAP note template is fully customizable, allowing you to tailor it to your specific needs. Whether you're a physician, nurse practitioner, or other healthcare provider, our template can help you streamline your documentation process, saving you time and ensuring accuracy.
Get Your SOAP Note Template
Download our SOAP note template today to improve your documentation accuracy and streamline your workflow. Our template is available in DOCX format and can be easily customized to suit your specific requirements. Ensure complete and consistent documentation of your patient encounters and improve patient outcomes. Visit BizzLibrary.com now to dowload this important document along with hundreds of other free templates!
Is the template content above helpful?
Thanks for letting us know!
Reviews
Shannan Luna(7/8/2023) - DEU
Grateful!!
Last modified
Our Latest Blog
- A Guide to Make a Business Plan That Really Works
- The Importance of Vehicle Inspections in Rent-to-Own Car Agreements
- Setting Up Your E-mail Marketing for Your Business: The Blueprint to Skyrocketing Engagement and Sales
- The Power of Document Templates: Enhancing Efficiency and Streamlining Workflows
Template Tags
Need help?
We are standing by to assist you. Please keep in mind we are not licensed attorneys and cannot address any legal related questions.
-
Chat
Online - Email
Send a message
You May Also Like
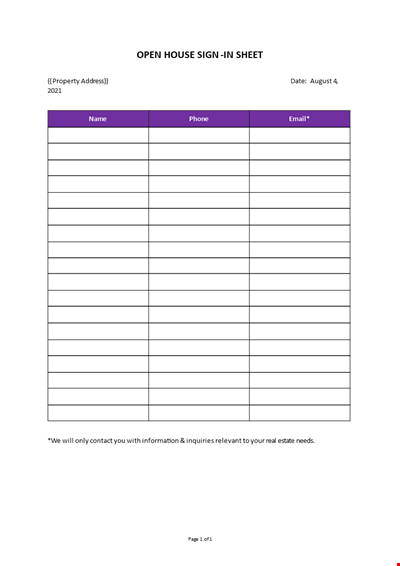
Open House Sign-in Sheet
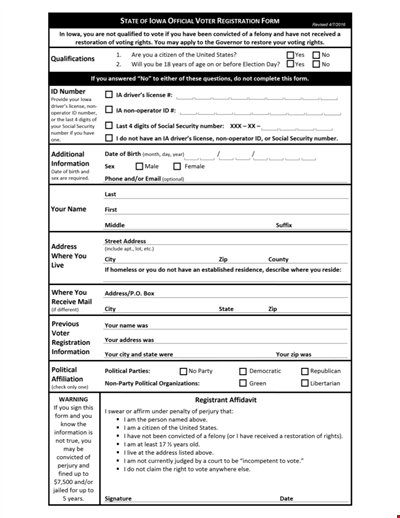
Printable Voter Registration Form

Department Material Requisition Form
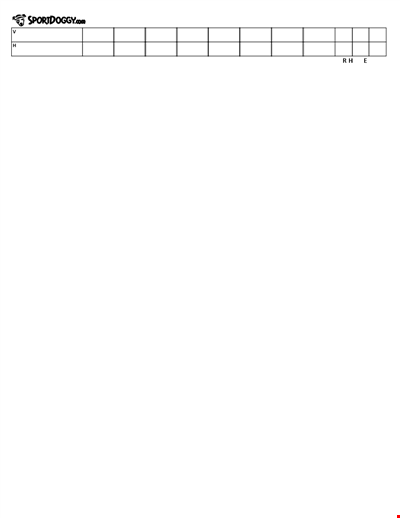
Softball Box Score Sheet Template - Track game stats efficiently
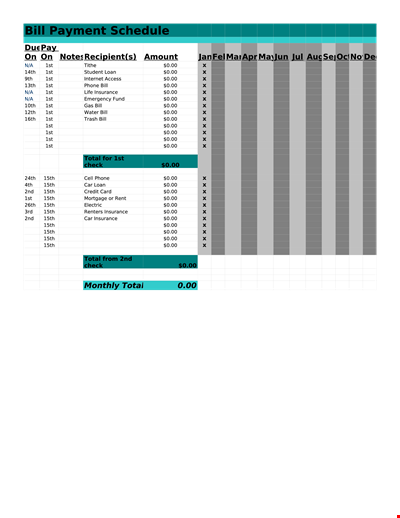
Manage Your Finances with Our Free Printable Bill Payment Schedule Template
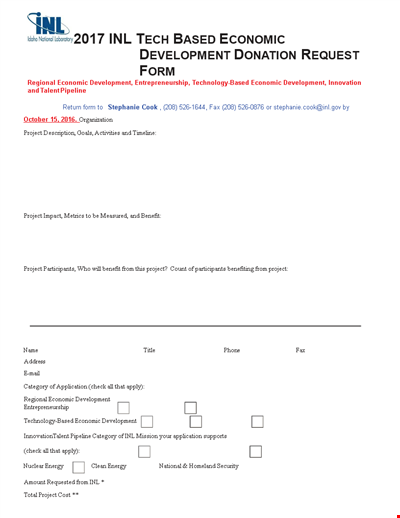
Tech-Based Economic Development Donation Request

Business Commercial Lease Rental Application Form - Apply for a Lease
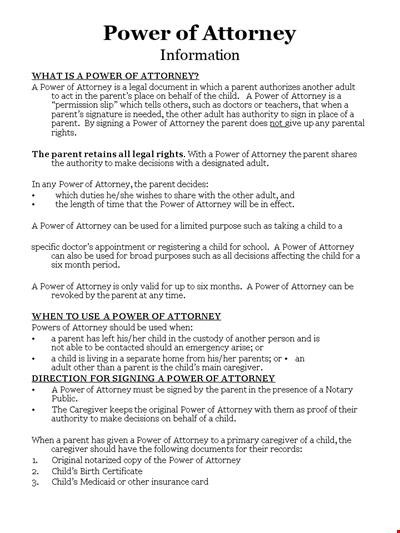
Child Medical Power of Attorney Form - Granting Parental Rights to Caregiver

Easter Social Media Post
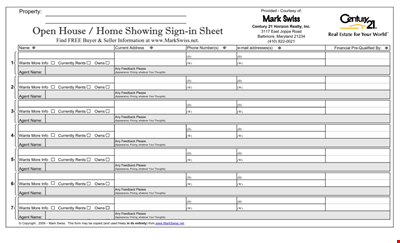
Get the Best Open House Showing Sign In Sheet Template Here
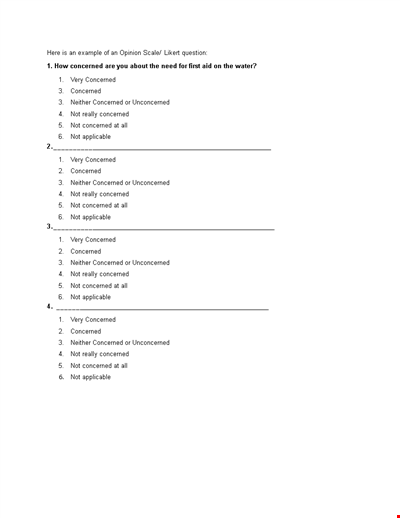
Understanding the Likert Scale: Neither Concerned nor Unconcerned
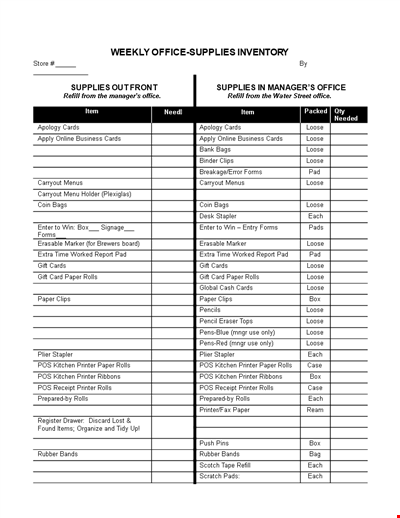
Weekly Office Supply Inventory List Example
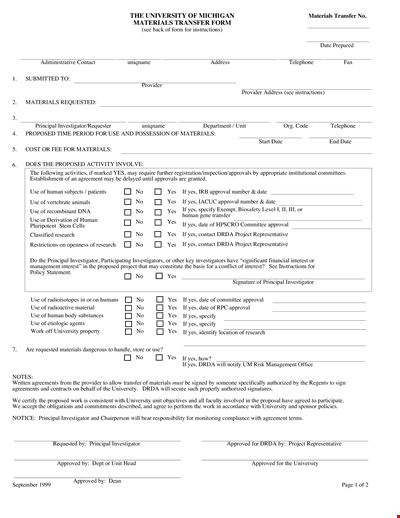
Material Transfer Form (University)

Design Work Order Form

Printable Large Oblique Graph Paper

Modern School Technology: Enhancing Education through Innovative Tools and Solutions